Yesterday afternoon Carolyn tucked me into bed. The zoledronic acid infusion I got Thursday at the hospital has left me feeling like I have a nasty flu combined with a smashing hangover. I fell asleep almost immediately but when I woke up I could hear the rain beating on our metal roof. I love that sound. Today, the dexamethasone is kicking in and it’s leaving me in a state of nervous fibrillation. I’ve never done speed, but I expect the sensation must be something like that. Now is a good time to write because I have this bizarre energy that needs an outlet. However, the dex gives me the shakes making it difficult to keep my fingers singly on the keys of my computer.
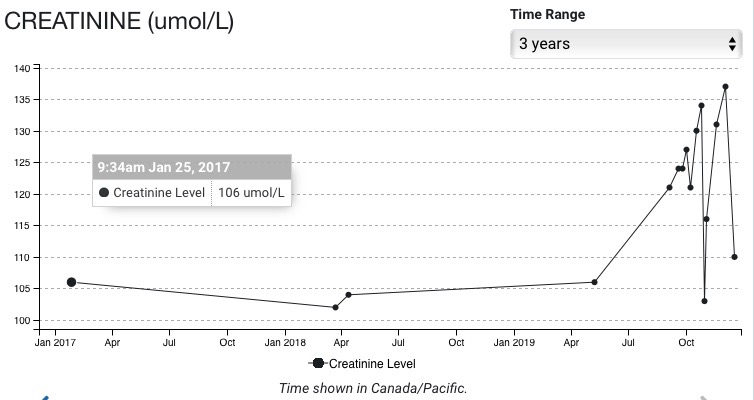
So, getting back to yesterday afternoon. Like I said I slept for some time and woke to the sound of rain pounding the metal roof. I just lay there. I find that lying in bed staring at the ceiling is not a bad way to pass the time. I could never do that before. I had the work ethic really bad when I was still gainfully employed and long after truth be told. Now, my body has taken charge of my reluctant mind and has forced me to sit still, to lie down and not feel guilty about it. Cancer has its upsides I guess, but I’m not sure that I fully subscribe to its methods. One thing for sure: There is no normal in my life anymore: sleep times vary, meals are still on schedule as are the ritual pill taking, but I can’t count on feeling the same way during each new cycle of chemotherapy that I felt on the previous one. Dex is predictable but the intensity of its effect varies. I only have to take it one more time on this course of chemo lasting until January. I start taking it again in late January when I start my second course of chemo with my fifth cycle. A course of chemo lasts approximately four weeks, a cycle, one week. At least that’s the pattern now. But I digress.
I’m lying on my bed focussed on the cedar beam that crosses the ceiling in the middle of our bedroom, light pouring in from the three windows just behind me at the head of the bed. I close my eyes and think about death. Well, more about dying than death, actually. It’s the process of dying that is absorbing me, not death itself which for too long we’ve considered the opposite of life. Dying is another thing altogether. Dying is the separation of consciousness and body. Consciousness in my estimation comes to an end at the point of death but my body, this collection of matter brought together by processes millions of years old, will immediately begin to become unglued. It loses its integrity as a collection of cells and begins to decompose, that is, to lose its composition.
I don’t have to tell you this. It’s hard to live for any length of time without coming across at least one death in the family, among friends, or by reading the news or obituaries on the local papers. We know about death although we don’t quite know what to make of it or how it pertains to us. It’s strange that for most of us we take for granted that ‘we’ don’t exist before our conception and birth and that ‘we’ become ‘we’ by a combination of hereditary traits, learned behaviour, and environmental factors. ‘We’ or ‘I’ are constructs. We are not born fully operational. We become ‘I’ over time, slowly developing personality traits, habits, and idiosycracies that define us as unique individuals. But we resist very strenuously the idea that if we come we must also go. But I digress again!
So, I’m back in my bedroom, lying on my back on my bed in that state of half sleep, very relaxed and I meditate. I meditate on my last breath. I’m thinking that dying is not much different than living. When we fall asleep and lose consciousness we have no idea whether we will awaken or not, we just take if for granted that we will. I’ve had two brothers-in-law die this past year. One died during the night in bed next to my sister. We say he died in his sleep. True enough. He wasn’t conscious when he took his last breath. Neither was my mother who died nearly two years ago, but she had demential and was so hopped up on morphine that I can’t say she died in her sleep. My sisters were there at the moment of her death. I missed it by a few hours. I was in pretty bad shape myself two years ago with symptoms on myeloma that went undiagnosed at the time. I was perennially exhausted, in a great deal of pain, and I couldn’t stand the vigil as my family surrounded my mom’s death bed waiting for her to take her last breath. I prefer to think of my dying as just another falling asleep kind of experience. My last one of course, but still.
Needless to say, there are only one or two ways of being born that I know of, but millions of ways to die. I like to think that my last breath will be in the comfort of home or at least in a hospice, somewhere nice. Many, many millions of people worldwide don’t die under such benign circumstances. Violent death is common. Five thousand Canadians die in vehicle crashes a year, fifty thousand Americans meet the same fate. I don’t fancy that as a way of dying, but if it’s quick, maybe. I can’t imagine being hacked to death with a machete after watching my family meet the same fate in 1994 Rwanda, or being shot by a stray bullet in Aleppo leaving me wounded and watching the blood spill out of me. No, give me a peaceful, quiet place to die.
I’ve been diagnosed with an incurable cancer but I’m told that it’s more like a chronic treatable condition than a CANCER that kills fast and unannounced. I’ve got some time to think about my last breath. I’m not sure if that’s good or bad. Certainly, I’ll roll with it. I remember clearly when I was a kid of twenty or so. I had a fairly serious back injury while working at a sawmill on Lulu Island and I needed back surgery to remove a disk in the lumbar area of my back. I was a kid in search of meaning in my life, not such an unusual thing. I remember lying in my hospital bed after the surgery, hanging over the edge puking my guts out and thinking to myself. I can milk this for everything it’s worth. I could stay on Compensation for a long time then go on disability or something along those lines. Or I could get out of the hospital and use this time to get my shit together. And that’s what I did. I got my shit together. I enrolled in the liberal arts program at Douglas College in New Westminster and never looked back. My injury allowed me time to think about my future without the pressure of work. That was luxurious, and it worked.
Now, I don’t need to get my shit together. It’s been together for a few decades and I’m happy with my shit. My encounter with cancer, in a way similar to my experience with my back surgery, is giving me time to think about my last breath, but to also remember that every breath I take until my last one is worth paying attention to and celebrating. Whatever I do until I take my last breath is not so important. Of course, I can’t help but do something and I will do things that have always mattered to me. It’s impossible to do nothing and still be alive. Even lying on the couch ‘doing nothing’ is doing something. Whatever I do will be the right thing at the time because it will be what I do. In any case it won’t matter one iota after I’m dead because ‘I’ won’t be around to care or experience regret or any other sentiment.