[WARNING: this post contains references to visualizations some might consider offensive, and I regress to being a potty-mouth. Be forewarned.]
I’m not feeling particularly creative, effusive or positive today. In fact, I’m feeling hard done by, angry and unhappy. Hence the title of this post. In fact, I’m feeling fucking crappy, as crappy as ever, or even more so, because for the last three weeks or so I’ve had a cold to compound the effects of my myeloma and the chemo meds I’m taking. Most of the time all I’ve been able to do is sleep, or stare out the windows.
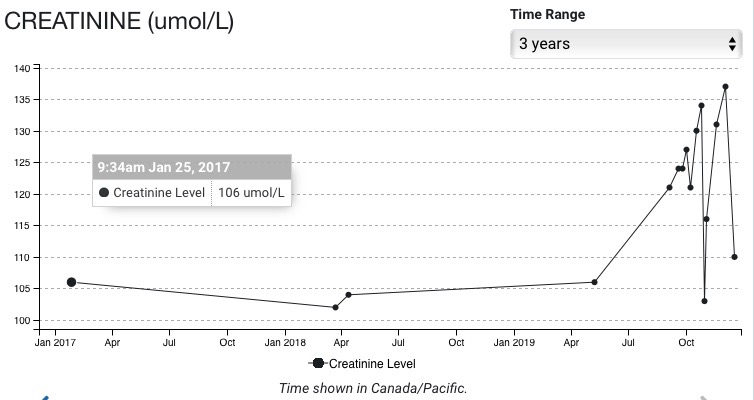
We just came back from the hospital an hour or so ago. Carolyn had to shovel huge piles of snow blocking our driveway and covering our truck just to get us there. Carolyn is my warrior! At the hospital, I got an injection of bortezomib (a proteasome inhibitor) into my abdomen and an infusion of zoledronic acid (a bone strengthening drug that has not-so-fun consequences for my kidney). They gave me 4 grams of zoledronic acid rather than the 3.5 I got last time. I have no idea why. They have a complex formula for deciding how much to give me including my weight and my lab results. Now, I’m just waiting for the chemo meds to kick the shit out of me as they surely will. At least dexamethasone gives me a bit of a boost of energy allowing me to carve a few words onto this ‘page’ out of my weary brain. The sculpture I’m carving I don’t feel is particularly elegant or fine, but my tools are dull so it’s what you get.
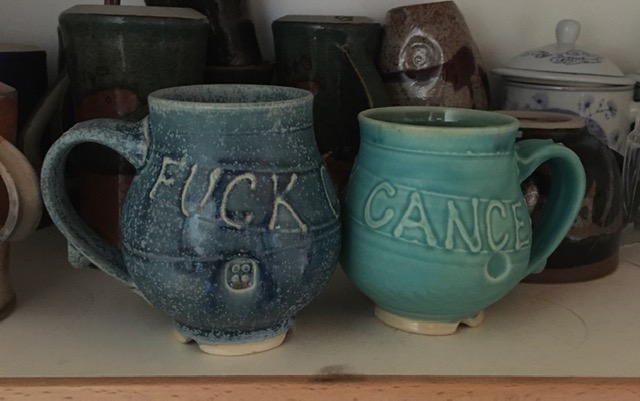
Do you like the mugs? Carolyn had them made by a very talented potter in the Valley who had previously made a set of mugs we bought from her that resemble these a lot except for the swear words.
Yeah, fuck cancer! I’m so sick and tired of being sick and tired! And now, to compound my shit, I have to worry about peripheral neuropathy. [I have complained about this before, but read about it again for fun.] I’ve had peripheral neuropathy for some time, many years actually. Peripheral neuropathy (PN) is a condition where the peripheral body parts, arms and legs to be precise, get to feeling numb, painful, and full of weird sensations like having bugs crawling all over them (something I’m feeling a lot at the moment). One of the side effects of the cocktail of chemo meds I’m taking is peripheral neuropathy. Left untreated it can lead to immobility, loss of sensation and life in a wheelchair. This is one of the nasty side effects of my meds, one that has forced a friend of mine who also has myeloma off this particular cocktail that’s often referred to as CyBorD. I’ve written about this before. I have to keep a close watch to determine whether or not the symptoms of PN are getting worse or not. It’s just one more thing to keep my mind occupied with my illness. Fuck cancer!
Did I say Fuck Cancer? Right, I did. And I mean it. I’m not sure what else I would prefer to die from, but cancer is not the companion I would have wished for on my way to the crematorium. Maybe a six-ton weight falling from the sky onto my head would be preferable, I don’t know. I have no way to assess the quality of various means of dying nor the means of communicating the results of any research I might do on the subject to you after the fact.
I may have already written about this…remember that brain fog is a classic side effect of anemia and myeloma, repetitiousness and forgetfulness probably are too… I read somewhere that an artist was asked if he wanted to be cremated or buried after he died. Instead of answering as you or I might he replied: “Surprise me!” Yeah, that’s the way I feel about it. I won’t be around to give a shit one way or another, but I have said I want to be cremated. I have had too many nasty dreams about being buried to want that as an option. Now, though, I’m starting to have moments when I visualize the crematorium attendant pushing my body into the furnace and my skin starting to cook like a pig on a spit as the fire gets hotter and hotter. I know, it’s gross and morbid. Sorry for bringing it up.
So, to change the subject, I’ve had a few moments of lucidity lately between bouts of feeling really nasty because of this cold, and I’m reading (in bed) about my ancestors here in Canada. My family goes back a long way as immigrants to Canada, back to early in the 18th Century actually on both my maternal and paternal sides. I’m finding out that my Norman ancestors called LeGuerrier (the warrior in French) were very likely actual warriors. A thousand years ago the Normans were highly trained and fierce warriors. They not only conquered England in 1066, but (I’ve just read) also became rulers in Sicily after they were invited there to help deal with an enemy. According to a book I’m reading they were often called on as mercenaries. One of the Norman rulers in Sicily was called Roger. His son Roger II took over after Roger I died and he was not known for his tender generosity. Roger that! In any case, the first Leguerrier in Canada can be traced back to 1748. He came earlier than that, but that date is the first mention of him in ‘the books’. He died a fairly old man. Infant mortality was very common then but so was death at any age. From what I’ve been reading living to reproductive age almost seems to have been the exception rather than the rule. These days I’m thinking about my ancestors, their lives and their deaths, and my place in the lineage. My grandpa Leguerrier died at the age of 76 in 1975 from stomach cancer if I remember correctly. My father died in 2007 at 96 years of age. We all come and go. Some of us live longer that others of the same generation but in the case of my grandpa Leguerrier and my father who were only fourteen years apart in age, I think I prefer to follow my grandpa’s lead because my father died after years of very poor quality of life, unable to feed himself because his hands were so distorted by arthritis. He was deaf, had been for years, and he was either in bed or in a wheelchair. To make matters worse, my mother had severe dementia and didn’t even recognize him on his deathbed. She was heard to point to him and say: “Who is that old man in the bed there anyway?” My mother died two years ago at 94 years of age. I can’t imagine she knew she was dying at the time. I’m not sure she knew that she was alive. Hey, wait a minute…